 0769-22660023
0769-22660023  0769-22660023
0769-22660023 In outpatient clinics, one often hears sighs like: “Doctor, my vision has been getting increasingly blurry lately. Is my presbyopia getting worse?” Or, “I'm getting older, my eyes aren't what they used to be—that's normal, right?”
Too many middle-aged and elderly individuals, especially our parents' generation, tend to attribute declining vision simply to “presbyopia,” overlooking the potential risks of serious underlying eye diseases. The eyes, especially the fundus, serve as a “window” to overall health and are also a “silent battlefield” for many blinding eye diseases.
Where is the fundus?
Clinically, the fundus refers to the internal structures of the eyeball behind the lens, including the retina, retinal blood vessels, optic disc, optic nerve fibers, the macula on the retina, and the choroid behind the retina.
The fundus is the only part of the body where arteries, veins, and capillaries can be directly observed with the naked eye. These vessels reflect systemic blood circulation and overall health status. Thus, numerous systemic diseases can manifest through fundus changes.
Hazards of Fundus Diseases
The primary harm of fundus diseases lies in diminished visual function, with severe cases potentially leading to blindness.
Many patients lack sufficient awareness of retinal diseases, misunderstanding their severity and delaying timely diagnosis and treatment. Symptoms like vision loss, narrowed visual fields, and floaters are often mistaken for cataracts or vitreous opacities. Allowing the condition to progress unchecked causes rapid deterioration of retinal function, leading to delayed treatment and loss of the optimal window for intervention.
Common Retinal Diseases
Retinal diseases are a primary cause of irreversible vision loss. They are not only diverse in type but also significantly impact visual acuity.
1. Macular Degeneration
The macula is a tiny central area of the retina that plays a crucial role in vision. Often referred to as the “heart of the retina,” it is responsible for the sharpest visual acuity in every individual.
When the macula becomes diseased, noticeable visual changes occur, such as abnormal color perception, blurred central vision, distorted or twisted images, and dimmed colors. These symptoms are relatively easy to detect. Once macular degeneration progresses to the point of central vision loss, reversal is nearly impossible. This is why severe macular degeneration is sometimes referred to as “eye cancer.”
Individuals over 50 experiencing vision loss should be vigilant for age-related macular degeneration. However, it's important to note that macular degeneration affects people of all ages.
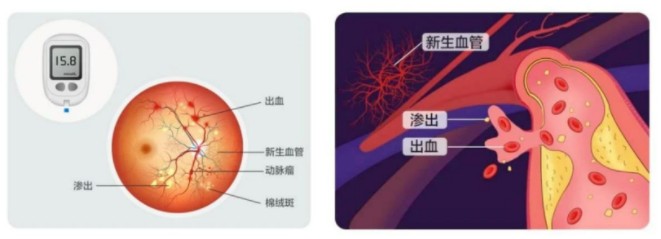
2. Diabetic Retinopathy
Diabetic retinopathy, also known as DR, is an eye disease that can lead to vision loss or even blindness. It has a high incidence rate and is common among diabetics with poorly controlled blood sugar.
Many diabetic patients with eye complications experience no obvious symptoms in the early stages—no redness, pain, itching, or bleeding—making it easy to overlook.
Patients often focus more on blood sugar control and managing systemic complications, neglecting retinal disease. However, once the condition progresses to advanced stages, treatment becomes not only costly but also unable to restore lost vision.
3. Central Retinal Artery Occlusion
Retinal artery occlusion, also known as “eye stroke,” occurs when the eye experiences a stroke. The risk factors for this condition mirror those of cerebral stroke—hypertension, hyperlipidemia, and cardiovascular/cerebrovascular diseases!
“Eye stroke” occurs suddenly and painlessly. If you experience blurred vision or sudden loss of vision in one eye—like a sudden blackout—seek immediate examination by an ophthalmologist.
The golden window for treating central retinal artery occlusion is 90 minutes. Beyond this timeframe, irreversible damage to retinal nerve tissue often occurs.
4. Rhegmatogenous Retinal Detachment
Among retinal diseases, rhegmatogenous retinal detachment is both common and highly complex. As the condition progresses, the detached area gradually expands. If it involves the macula, severe vision loss occurs, potentially leading to complete blindness and eye atrophy.
Who Needs Fundus Examinations?
Elderly Individuals
Age-related eye conditions such as posterior vitreous detachment, macular holes, retinal vein occlusion, and age-related macular degeneration may develop during the aging process. Regular examinations facilitate early detection and intervention to prevent blindness.
Diabetic patients
Diabetics should undergo regular examinations at the ophthalmology department. If retinal lesions are detected, early intervention through laser treatment or medication is essential. Even patients with no initial signs of diabetic retinopathy should have at least one annual eye examination.
High myopia patients
With the increasing prevalence of myopia, its detrimental effects on the retina cannot be overlooked, particularly in cases of high myopia exceeding 600 degrees.
High myopia causes elongation of the eyeball, leading to a series of retinal changes such as retinal detachment, macular schisis, macular holes, retinal-choroidal atrophy, and choroidal neovascularization. These conditions can severely impair vision and even pose a risk of blindness.
Individuals with high myopia should avoid strenuous physical activities and undergo regular dilated fundus examinations to detect potential risks like peripheral retinal degeneration or retinal tears.
Hypertensive Patients
Approximately 70% of hypertensive patients develop hypertensive retinopathy, closely linked to age and blood pressure control.
Early-stage hypertensive retinopathy often presents no obvious clinical symptoms. All hypertensive patients are advised to undergo comprehensive annual fundus examinations to detect retinal abnormalities promptly and initiate treatment early.